Position statement of the Brazilian Society of Clinical Analysis (SBAC) on the report of the presence of spermatozoa in urine samples – 2024
Posicionamento da Sociedade Brasileira de Análises Clínicas (SBAC) sobre o relato da presença de espermatozoides em amostra de urina – 2024
Mauren Isfer Anghebem1, Ana Paula Giolo Franz2, Flávia Martinello3
1 Farmacêutica, Doutora em Ciências Farmacêuticas/Análises Clínicas, Professora Adjunta da Escola de Medicina e Ciências da Vida da Pontifícia Universidade Católica e Professora Adjunta do Departamento de Análises Clínicas da Universidade Federal do Paraná/UFPR, Curitiba – Paraná – Brasil. Membro do Grupo Técnico-Científico da Sociedade Brasileira de Análises Clínicas – SBAC.
2 Biomédica, Doutoranda em Bioexperimentação, Laboratório de Análises Clínicas do Hospital de Clínicas de Passo Fundo, Passo Fundo-RS, Brasil. Membro do Grupo Técnico-Científico da Sociedade Brasileira de Análises Clínicas – SBAC.
3 Farmacêutica, Pós-doutora em Análises Clínicas, Professora do Departamento de Análises Clínicas da Universidade Federal de Santa Catarina/UFSC, Florianópolis – Santa Catarina – Brasil. Membro do Grupo Técnico-Científico da Sociedade Brasileira de Análises Clínicas – SBAC.
INTRODUCTION
Urinalysis is an important diagnostic tool. The results of this examination, when analyzed in conjunction with the patient’s medical history and physical examination, can diagnose and monitor urinary system diseases, metabolic disorders, and infectious conditions, even in asymptomatic patients. (1)
Urinalysis comprises three main phases: pre-analytical, analytical, and post-analytical. The pre-analytical phase is essential to ensure accurate results and reduce sample rejection and recollection. In this regard, the clinical laboratory is responsible for providing the patient with detailed information regarding preparation and urine sample collection procedures. It should be emphasized to the patient that factors such as diet, hydration, diuresis, medication use, physical exercise, and sexual activity prior to sample collection may interfere with the urinalysis results. (2)
In males, urine samples collected after sexual intercourse or masturbation may contain spermatozoa that remained in the urethra, without clinical significance. However, the presence of spermatozoa in urine may also be associated with certain diseases or the use of specific medications, which is why its documentation in the reports of adult males is relevant. (3) In urine samples from females, the presence of these elements requires caution and specific measures, which are discussed below.
Spermatozoa in the urine of adult males
Spermatozoa are commonly observed in the first post-ejaculatory urination, regardless of the patient’s age. In older males, spermatozoa can also be found in the urine due to reduced contraction of the internal urethral sphincter. (3) In both conditions, the presence of these elements has no clinical significance.
Seminal fluid can therefore contaminate urine both after normal ejaculation and in cases of retrograde ejaculation. Retrograde ejaculation is a disorder resulting from anatomical, traumatic, neuropathic, and/or pharmacological conditions, characterized by the reverse flow of seminal fluid from the posterior urethra into the bladder during ejaculation, potentially leading to male infertility. (4)
Although the presence of spermatozoa in urine is not conclusive, it is an important factor in the diagnosis of retrograde ejaculation. Testing for spermatozoa in post-ejaculatory urine to determine the presence of partial retrograde ejaculation is recommended in infertile patients with low semen volume. (5)
Retrograde ejaculation most commonly occurs as a result of transurethral prostatectomy, retroperitoneal lymph node dissection, and diabetic neuropathy. Diabetic neuropathy contributes to a broad spectrum of clinical disorders, including ejaculatory disorders, which is why spermatozoa can be found in the urine of individuals with diabetes. Retrograde ejaculation can also be associated with a history of pelvic surgery for colorectal cancer or transurethral resection of the prostate, due to nerve damage involved in ejaculation during the surgical procedure. Additionally, spermatozoa may be found in the urine of individuals using alpha-blockers or selective serotonin reuptake inhibitors, which are known risk factors for ejaculatory disorders. (6) Spermatozoa can also be observed in the urine of individuals who use psychoactive drugs and alcohol, as these substances affect the closure of the internal urethral sphincter during ejaculation, facilitating the flow of semen into the bladder. (3)
Spermatozoa in the urine of male children and adolescents
Semenarche or spermarche is the term used to describe a boy’s first ejaculation, a spontaneous release of semen that typically occurs around 12 or 13 years of age. This involuntary event usually happens during sleep and is referred to as a nocturnal emission. It is a normal physiological process, which is why, starting from this age, spermatozoa can be found in the urine of male adolescents, even if they have not engaged in sexual intercourse or masturbation in the hours prior to urine sample collection.(7) Spermaturia is a common and regular event during the early and middle stages of puberty and may occur before any other sign of puberty, making it a useful indicator for determining gonadal maturation.(8) Thus, it is up to the attending physician to determine the clinical relevance and the need for testing spermatozoa in the urine of male children and adolescents.
Spermatozoa in the urine of adult females
The observation of spermatozoa in the urine of adult females is associated with recent sexual exposure, indicating a failure in the pre-analytical phase of urinalysis. The presence of these elements in the urine of this population is only relevant in forensic contexts, where there is suspicion of sexual abuse or other forms of non-consensual exposure. Only in this specific situation, under judicial request, should the testing for spermatozoa in urine be performed, and its presence must be mandatorily reported. In such cases, all stages of the chain of custody must be ensured. The chain of custody defines the entire path of the material evidence, from its recognition to its disposal, with the aim of guaranteeing the authenticity, integrity, and preservation of the evidence.
Spermatozoa in the urine of female children and adolescents
The finding of spermatozoa in the urine of female children and adolescents requires the investigation of possible pre-analytical errors. The clinical laboratory must ensure the quality of all stages of the examination, including traceability, to avoid and rule out possible sample mix-ups or contamination during the collection and/or processing of the sample.
According to Decree-Law number 2,848/40 (Brazilian Criminal Code), Article 217-A, it is considered a crime to have carnal conjunction or practice libidinous acts with a minor under 14 years of age. (9) Therefore, once the quality of the sample is guaranteed, the observation of spermatozoa in the urine of female children and adolescents under 14 years of age may characterize sexual abuse and should always be reported in the urine examination report. Furthermore, the laboratory must notify the Guardianship Council or the Childhood and Youth Court or the Public Prosecutor’s Office, in the absence of the former. This action is in line with Opinion number 18/2024,(10) of the Brazilian Federal Council of Medicine (CFM), published on July 27, 2024, which states that it constitutes omission and negligence not to report in the urine examination report the presence of spermatozoa in female patients up to 13 years, 11 months, and 29 days old.
According to Article 245 of the Brazilian Child and Adolescent’s Statute (ECA), a physician or person responsible for a healthcare facility who fails to report to the competent authority cases of which they have knowledge, involving suspicion or confirmation of mistreatment against a child or adolescent, commits an administrative infraction subject to a fine.(11) According to the CFM, “notification to the Guardianship Council by the physician or person responsible for the healthcare facility is, therefore, mandatory in cases of suspected or confirmed sexual abuse against children and adolescents up to 13 years, 11 months, and 29 days old, under penalty of a fine and double fine in case of recurrence. All samples from female children and adolescents up to 13 years, 11 months, and 29 days old in which the presence of spermatozoa has been detected should be stored under appropriate conditions for possible forensic studies. The Guardianship Council usually provides a standard form for notifications, which may vary according to the state.”(10)
FINAL CONSIDERATIONS
The pre-analytical phase, which encompasses patient orientation and preparation, sample collection, transport, and storage, plays a crucial role in the accuracy of laboratory results and must be rigorously controlled to ensure the validity of the data.
Sexual intercourse should be avoided one day prior to urine sample collection due to the likelihood of sample contamination with proteins and other elements, such as epithelial cells and spermatozoa. It is essential to reinforce guidance to patients to discard the first urine stream, promoting the elimination of elements normally present at the urethral opening. This also minimizes the chances of the urine sample being contaminated by spermatozoa that remain in the urethra.
Although the literature has largely focused on adult males, the presence of spermatozoa in urine samples from other populations must be carefully evaluated due to clinical and legal implications.
The CFM Opinion number 18/2024(10), which recommends reporting the finding of spermatozoa in the urine of female children and adolescents up to 13 years, 11 months, and 29 days of age, is directed to laboratories run by physicians and regularly registered with the Regional Medical Councils. However, it may also be followed by clinical analysis laboratories under the technical responsibility of other professionals legally qualified to perform clinical analyses.
The reporting of the presence of spermatozoa in the urine of male children and adolescents is at the discretion of the laboratory. However, it is recommended that it be reported so that the attending physician can determine the clinical relevance of the finding.
In urine samples from individuals aged 14 years or older, it is not advisable to report the presence of spermatozoa due to the lack of clinical relevance. In these cases, the rejection of the sample with a request for a new collection may be indicated and standardized by the laboratory to ensure a sample free from seminal material interference. It is important for the laboratory to have well-established procedures that guarantee the entire chain of custody in cases under judicial request.
It is emphasized that, in this document, the term “sex” is defined by the anatomical aspects (genitalia) of the human species; thus, the term has been used to refer to the gender, male or female, assigned at birth.(12)
RECOMMENDATIONS FROM SBAC
The SBAC recommends that:
- In the event of unequivocal observation of spermatozoa in the urine, laboratories should follow the algorithm illustrated in Figure 1.
- Clinical analysis laboratories should request a Consent Form for the reporting of all elements observed in the urinalysis and include the observations described in Figure 1.
- Laboratories should implement detailed procedures with a flow for notifying cases of urine samples from female children and adolescents under 14 years of age with the presence of spermatozoa to Guardianship Council, according to their routine, safeguarding against ethical and criminal penalties.
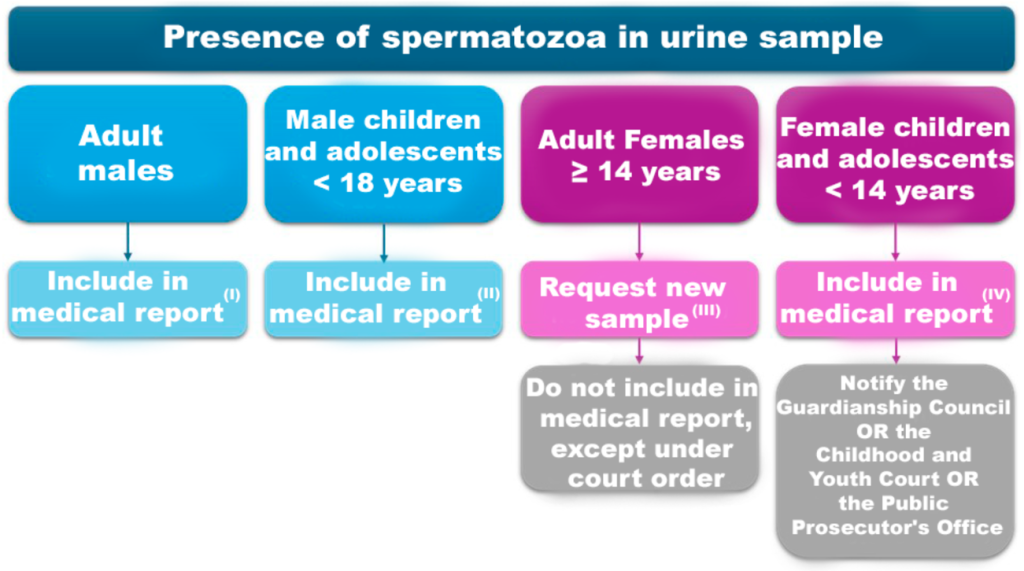
Figure 1
Algorithm for reporting the presence of spermatozoa in urine in the laboratory report.
Notes:
The comments I, II, III, and IV below may be used as explanatory notes in urinalysis reports.
(I) Spermatozoa may be observed in post-ejaculatory urine, regardless of the patient’s age; and in older adults, due to reduced contraction of the internal urethral sphincter, without clinical relevance.(1) The presence of spermatozoa may also be associated with retrograde ejaculation, which consists of the reverse flow of seminal fluid from the posterior urethra into the bladder during ejaculation, resulting from anatomical, traumatic, neuropathic, and/or pharmacological conditions. Interpretation is at the discretion of the physician.(2)
1 Tomita M, Kikuchi E, Maeda T, Kabeya Y, Katsuki T, Oikawa Y, Kato K, Ohashi M, Nakamura S, Oya M, Shimada A. Clinical Background of Patients with Sperm in Their Urinary Sediment. PLoS One. 2015 Sep 11;10(9):e0136844.
2 Gupta S, Sharma R, Agarwal A, Parekh N, Finelli R, Shah R, et al. A Comprehensive Guide to Sperm Recovery in Infertile Men with Retrograde Ejaculation. World J Mens Health. 2022 Apr;40(2):208-216. doi: 10.5534/wjmh.210069.
(II) The reporting of the presence of spermatozoa in the urine of male children and adolescents may be useful in determining gonadal maturation, with the clinical relevance of the finding left to the physician’s discretion.(1)
1 Engelbertz F, Korda JB, Engelmann U, Rothschild M, Banaschak S. Longevity of spermatozoa in the post-ejaculatory urine of fertile men. Forensic Sci Int. 2010 Jan 30;194(1-3):15-9.
(III) The laboratory may establish criteria for rejection and request a new sample when observing the presence of spermatozoa in urine samples from individuals aged over 14 years.
(IV) The presence of spermatozoa in urine samples from children and adolescents under 14 years of age will be reported in the laboratory report and notified to Guardianship Council or to the Childhood and Youth Court or to the Public Prosecutor’s Office, in accordance with Law No. 8,069/90 (Brazilian Child and Adolescent’s Statute (ECA)(1) and Decree-Law number 2,848/40 (Criminal Code)(2) , under the risk of criminal infringement.
1 Brasil. Lei nº 8.069, de 13 de julho de 1990. Dispõe sobre o Estatuto da Criança e do Adolescente e dá outras providências. Diário Oficial da União, 27 set. 1990.7.
2 Brasil. Decreto-Lei nº 2.848, de 7 de dezembro de 1940. Código Penal. Diário Oficial da União, 3 jan. 1941.
REFERENCES
- Haq K, Patel DM. Urinalysis: Interpretation and Clinical Correlations. Med Clin North Am. 2023 Jul;107(4):659-679.
- Coppens A, Speeckaert M, Delanghe J. The pre-analytical challenges of routine urinalysis. Acta Clin Belg. 2010 May-Jun;65(3):182-9.
- Tomita M, Kikuchi E, Maeda T, Kabeya Y, Katsuki T, Oikawa Y, Kato K, Ohashi M, Nakamura S, Oya M, Shimada A. Clinical Background of Patients with Sperm in Their Urinary Sediment. PLoS One. 2015 Sep 11;10(9):e0136844.
- Gupta S, Sharma R, Agarwal A, Parekh N, Finelli R, Shah R, et al. A Comprehensive Guide to Sperm Recovery in Infertile Men with Retrograde Ejaculation. World J Mens Health. 2022 Apr;40(2):208-216.
- Mieusset R, Walschaerts M, Isus F, Almont T, Daudin M, Hamdi SM. Diagnosis of Partial Retrograde Ejaculation in Non-Azoospermic Infertile Men with Low Semen Volume. PLoS One. 2017 Jan 6;12(1):e0168742.
- Ariagno JI, Mendeluk GR, Pugliese MN, Sardi SL, Acuña C, Repetto HE, Curi SM. The only presence of sperm in urine does not imply retrograde ejaculation. Arch Androl. 2005 Nov-Dec;51(6):431-6.
- Pedersen JL, Nysom K, Jørgensen M, Nielsen CT, Müller J, Keiding N, Skakkebaek NE. Spermaturia and puberty. Arch Dis Child. 1993 Sep;69(3):384-7.
- Engelbertz F, Korda JB, Engelmann U, Rothschild M, Banaschak S. Longevity of spermatozoa in the post-ejaculatory urine of fertile men. Forensic Sci Int. 2010 Jan 30;194(1-3):15-9.
- Brasil. Decreto-Lei nº 2.848, de 7 de dezembro de 1940. Código Penal. Diário Oficial da União, 3 jan. 1941.
- Conselho Federal de Medicina. Parecer CFM nº 18/2024, de 27 de julho de 2024. Available at: https://sistemas.cfm.org.br/normas/visualizar/pareceres/BR/2024/18.
- Brasil. Lei nº 8.069, de 13 de julho de 1990. Dispõe sobre o Estatuto da Criança e do Adolescente e dá outras providências. Diário Oficial da União, 27 set. 1990.
- Posicionamento Conjunto Medicina Diagnóstica Inclusiva: cuidado de pacientes transgênero. SBEM, CBR, SBPC-ML, 2019.
This position should be cited as:
Anghebem, Mauren Isfer; Franz, Ana Paula Giolo; Martinello, Flávia. Position statement of the Brazilian Society of Clinical Analysis (SBAC) on the report of the presence of spermatozoa in urine samples – 2024. Comissão de Publicações da Sociedade Brasileira de Análises Clínicas – SBAC. RBAC. 2024; 56(3):138-142.
